Is this year’s flu season taking an unexpected toll on public health? With restrictions easing after years of stringent COVID-19 measures, the 2022-2023 flu season has intensified, spreading rapidly across 43 states. Alarming statistics reveal approximately 9.1 million flu cases, 110,000 hospitalizations, and 4,700 deaths to date, including 17 pediatric deaths. This analysis delves into the severity of the current flu season, examining contributing factors like diminished herd immunity and widespread viral transmission patterns. Understanding these dynamics provides critical insight into navigating the formidable challenges presented by this year's flu outbreak.
Understanding the Severity of the Flu Season in 2023

The severity of the 2022-2023 flu season is pronounced, primarily due to the relaxation of COVID-19 protective measures that previously mitigated flu transmission. With fewer restrictions on social gatherings and mask-wearing, the flu virus has had more opportunities to spread. This has resulted in heightened flu activity across the United States, with 43 states reporting high or very high levels of flu cases. As the flu circulates more freely, it poses a greater risk to public health, particularly affecting vulnerable populations.
This flu season's impact is underscored by significant numbers in both morbidity and mortality. Approximately 9.1 million flu illnesses have been recorded, leading to 110,000 hospitalizations. The virus has claimed 4,700 lives, including 17 pediatric deaths. These statistics reflect the substantial burden on healthcare systems and the urgent need for effective public health interventions to reduce transmission and manage severe cases. The high incidence of severe outcomes underscores the importance of understanding and addressing the factors that contribute to this year's flu season severity.
The widespread nature of this flu season can be attributed to the virus's increased transmission in communities. With the easing of COVID-19 precautions, individuals are more prone to contracting the flu, emphasizing the necessity for continued vigilance and preventive measures. Public health agencies are urged to promote vaccination and proactive health behaviors to mitigate the ongoing impact of the flu season. The following table summarizes the critical metrics that illustrate the flu season's severity:
| Metric | Data |
|———————|—————|
| Flu Illnesses | 9.1 million |
| Hospitalizations | 110,000 |
| Deaths | 4,700 |
| Pediatric Deaths | 17 |
Comparing Current Flu Season with Previous Years

The 2022-2023 flu season, while severe, does not yet match the catastrophic impact of the 2017-2018 flu season, which remains the deadliest on record with 80,000 fatalities. This year, there have been approximately 4,700 deaths so far, indicating a significant public health challenge but on a lesser scale than seen in 2017-2018. The current season's severity is highlighted by the high number of illnesses and hospitalizations, yet it is crucial to acknowledge that the death toll has not reached the unprecedented levels of the 2017-2018 outbreak. The difference underscores the importance of ongoing preventive measures and medical interventions to curb the spread and impact of the flu.
In comparison to last year's flu season, the 2022-2023 period is peaking later, despite maintaining high activity levels across the majority of the United States. The delayed peak this season suggests that the flu might remain a persistent threat for weeks longer than anticipated, stressing the need for continued vigilance. This shift in timing may be attributed to variations in virus strains and public health responses, which have influenced transmission patterns. Health officials remain focused on monitoring the flu's progression and adapting strategies to mitigate its effects.
- The 2022-2023 flu season has fewer deaths compared to the 2017-2018 season.
- Current flu activity is peaking later than last year.
- High flu activity levels are expected to persist longer this year.
- The death toll in the current season is significantly lower than the record-high 2017-2018 numbers.
Regional Differences in Flu Impact
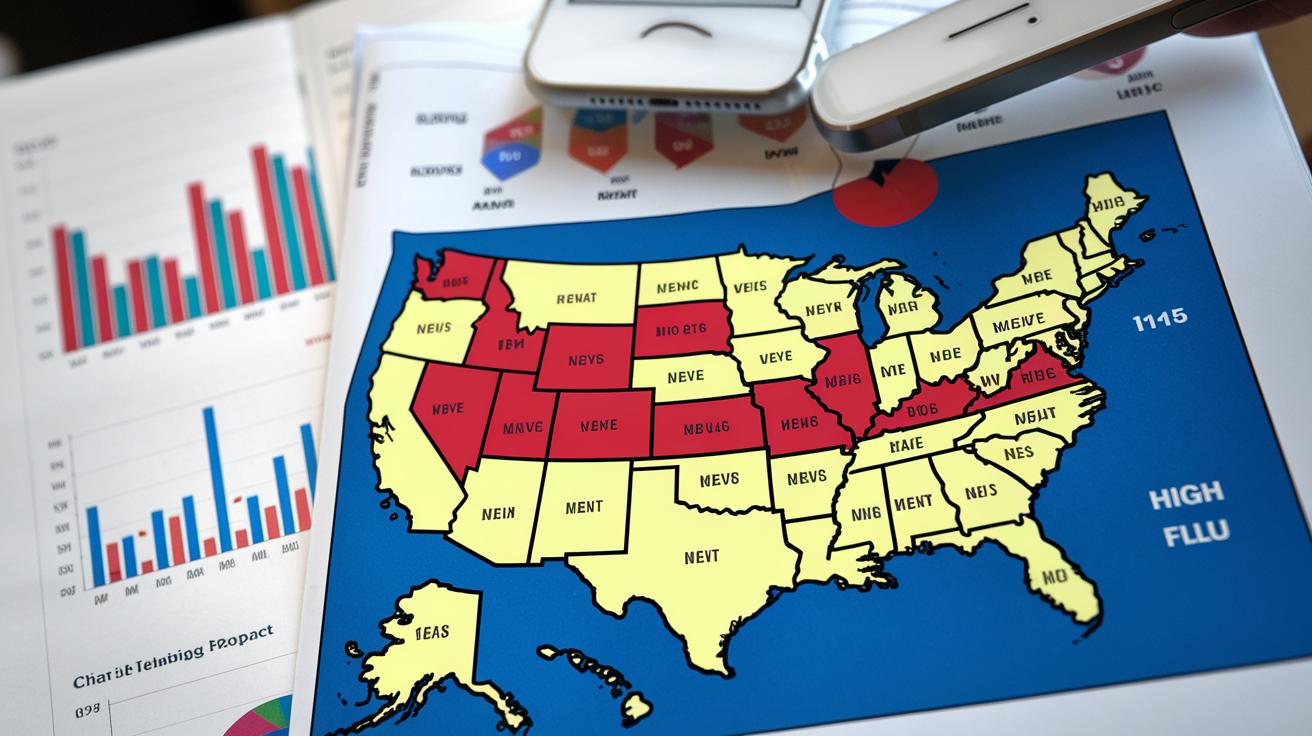
How is flu activity distributed across the United States? With 43 states currently reporting high or very high flu activity, the widespread transmission is evident, impacting regions differently based on various factors. The northeastern and midwestern states have experienced particularly high flu prevalence, attributed in part to dense urban populations and colder climates that facilitate indoor gatherings. In contrast, states with milder weather patterns, such as some in the southern regions, display variable flu activity levels, reflecting regional differences in public health preparedness and community response.
What factors influence flu transmission in different regions? Several key elements contribute to the variability in flu impact across states:
- Local Public Health Strategies: Differing vaccination campaigns and public health advisories can significantly alter flu transmission rates.
- Population Density: High-density areas often experience faster spread due to more frequent close contact among individuals.
- Healthcare Infrastructure: Regions with robust healthcare systems can better manage outbreaks and provide timely interventions.
- Climate and Seasonal Variability: Colder regions may see higher flu activity due to increased indoor activities, which elevate transmission risks.
- Community Compliance with Health Guidelines: Adherence to preventive measures, such as mask-wearing and social distancing, varies across regions, influencing flu spread.
How do these factors shape flu transmission patterns? The interplay of these regional factors creates diverse transmission dynamics across the country. In areas with strong public health infrastructure and high vaccination rates, the flu's impact may be mitigated, leading to lower incidence rates and fewer complications. Conversely, regions with fewer resources or lower compliance with preventive measures may experience more pronounced flu outbreaks, stressing local healthcare systems. Recognizing these variations is crucial for tailoring public health responses and allocating resources effectively to combat the flu.
Expert Recommendations and Public Health Advisories

How important is flu vaccination this year? According to experts, vaccination remains a critical measure in combating the ongoing flu season. An internal medicine specialist highlights that it is not too late to receive a flu shot, as flu activity is expected to continue for several weeks. The Centers for Disease Control and Prevention (CDC) originally recommended receiving the vaccine by the end of October to maximize protection before peak flu activity. However, given the current high levels of flu transmission, vaccination can still offer significant protection, reducing the risk of severe illness and hospitalization.
What proactive measures can be taken to protect against the flu? In addition to vaccination, several health strategies are advised to minimize flu transmission. Public health advisories emphasize the importance of combining vaccination with other preventive actions to bolster defenses against the virus. The CDC suggests the following flu prevention tips:
- Get vaccinated annually to maintain immunity against prevalent flu strains.
- Practice good hygiene by washing hands frequently and using hand sanitizers.
- Avoid close contact with sick individuals to reduce the risk of catching the flu.
- Stay home when experiencing flu symptoms to prevent spreading the virus to others.
By adhering to these recommendations, individuals can significantly lower their chances of contracting and spreading the flu, contributing to broader public health efforts to control the current flu season's impact.
The Role of Vaccination in Controlling Flu Season Severity

Why is an annual flu vaccination necessary? The flu virus undergoes frequent changes, necessitating yearly updates to the vaccine to combat the most prevalent strains effectively. Immunity from the flu vaccine diminishes over time, which means that without annual vaccination, individuals become increasingly susceptible to new virus variants each season. This annual vaccination ensures the immune system is primed to recognize and fight off the flu virus, thus playing a critical role in reducing the spread and severity of influenza outbreaks.
How effective are vaccination campaigns in reducing flu cases? Vaccination campaigns are instrumental in curbing the incidence and severity of flu cases. These campaigns aim to increase vaccination rates by raising awareness about the benefits and necessity of the flu shot, promoting accessibility through clinics and pharmacies, and addressing public misconceptions about vaccine safety and efficacy. By achieving high vaccination rates, these campaigns significantly reduce the number of flu cases, hospitalizations, and deaths, thereby alleviating the burden on healthcare systems and protecting vulnerable populations.
| Vaccine Feature | Impact |
|————————-|——————————————————|
| Annual Update | Targets the most prevalent flu strains each season |
| Diminishing Immunity | Necessitates yearly vaccination for ongoing protection |
| Campaign Effectiveness | Reduces flu cases and healthcare burden |
| Public Awareness | Increases vaccination rates and addresses misconceptions |
Vaccination remains a cornerstone of public health strategy, especially during severe flu seasons, by mitigating the virus's transmission and impact.
Addressing Common Flu Myths and Misconceptions
Common misconceptions about the flu contribute to widespread misunderstanding of the virus and its impact on public health. A prevalent myth is that the flu is merely a severe cold, which undermines the potential severity of influenza. Another misconception is that healthy individuals do not need flu vaccination, ignoring the community-wide benefits of herd immunity and personal protection against severe outcomes. Such myths can hinder effective prevention and control measures, exacerbating the flu's spread and impact.
- Myth: The flu is just a severe cold.
Fact: Influenza can cause a range of illnesses from mild to deadly, affecting the nose, throat, and lungs.
- Myth: Healthy people do not need a flu vaccine.
Fact: Everyone over six months should get vaccinated to protect themselves and reduce transmission.
- Myth: The flu vaccine causes the flu.
Fact: The vaccine is made from inactivated virus, which cannot cause influenza.
- Myth: Annual vaccination is unnecessary.
Fact: Flu virus strains change yearly, necessitating updated vaccines for effective protection.
Final Words
Amidst the current flu season's severity, relaxation of previous COVID-19 measures has significantly contributed to increased flu transmission. This season, marked by high activity in 43 states, has resulted in substantial illnesses, hospitalizations, and fatalities. Comparing to past seasons like 2017-2018, which was notoriously deadly, this year's late peak raises concern, yet offers a window for interventions.
Effective regional strategies and vaccination campaigns are crucial. Vaccination, emphasized as a proactive measure, remains vital in mitigating impacts. The ongoing effort against flu misconceptions highlights the importance of evidence-based understanding. Addressing how bad is flu season this year, public health measures and informed strategies will be essential in navigating its challenges, fostering resilience and health protection.
FAQ
What are the CDC guidelines for influenza in 2023?
The CDC provides guidelines recommending annual flu vaccinations and advises on best practices for preventing flu spread, such as hand hygiene and avoiding close contact with sick individuals.
How severe is the flu this year?
The severity of the flu this year is significant, with 43 states reporting high or very high activity, and approximately 9.1 million flu illnesses recorded so far, indicating increased severity over previous seasons.
Why is the flu season particularly bad this year?
This year's flu season is severe due to the relaxation of COVID-19 protective measures, leading to increased transmission and higher flu activity across numerous states compared to previous years.
When is flu season typically the worst?
Flu season usually peaks between December and February, with varying activities and severity influenced by factors such as public health policies and vaccination rates.
How safe is the flu shot in 2023?
The flu shot is considered safe, with annual updates targeting prevalent strains to enhance effectiveness, and experts still recommend vaccination even late in the season to reduce illness severity.