Is the flu shot worth the annual hassle, or is it just another medical recommendation to overlook? As flu season looms, this question hovers in the minds of many concerned individuals. With updated data showing the flu shot significantly curtails the risk of flu and its complications, it's essential to assess its value accurately. The CDC continues to advocate for the vaccine as the most effective defense against influenza. Understanding its effectiveness across different age demographics and awareness of its benefits and risks allows for informed decisions. Let's explore whether the flu shot deserves its prominence in public health discussions.
Understanding the Effectiveness of the Flu Shot

Updated flu vaccines play a critical role in combating influenza by targeting the most prevalent virus strains each year. This annual update is essential because the influenza virus mutates, necessitating a vaccine that is tailored to the current viral landscape. The Centers for Disease Control and Prevention (CDC) consistently reports that the flu vaccine is the most effective method for preventing influenza and its related complications.
The flu shot substantially reduces the risk of contracting influenza and minimizes the severity of symptoms if the virus is contracted. By priming the immune system with an inactivated or weakened form of the virus, the vaccine enables the body to mount a robust defense, significantly lowering the likelihood of severe outcomes, such as hospitalization or death.
- Vaccine effectiveness for children: Children benefit significantly from vaccination, with studies showing reduced incidence and severity of flu-related illnesses.
- Vaccine effectiveness for adults: For adults, the flu shot decreases the risk of flu-related complications and work absenteeism.
- Vaccine effectiveness for seniors: Seniors, who are more susceptible to severe flu outcomes, receive tailored vaccines that offer enhanced protection.
- General efficacy studies on flu vaccine: Efficacy studies indicate that vaccinated individuals have a lower incidence of flu, reduced severity of symptoms, and a decrease in flu-related complications.
Annual flu vaccine updates are informed by global surveillance data identifying circulating strains. Efficacy studies and data collection ensure that vaccines remain effective and relevant. Despite variations in yearly effectiveness due to viral changes, the overwhelming consensus is that the flu shot remains a crucial preventative measure, offering significant protection across diverse demographics.
Benefits of Getting the Flu Shot

The flu shot's life-saving potential lies in its ability to prevent severe complications such as dehydration, exacerbation of chronic conditions, and secondary infections like bacterial pneumonia. By stimulating an immune response, the vaccine significantly diminishes the risk of hospitalization and mortality associated with influenza-related complications. This preventive measure is particularly crucial for vulnerable populations, including the elderly, young children, and individuals with pre-existing health conditions.
- Prevention of severe flu complications: The flu shot reduces the likelihood of life-threatening complications and hospitalizations.
- Reduction in sick days: Annual vaccination cuts down the number of influenza-related sick days, preserving productivity levels.
- Contribution to herd immunity: Vaccination helps protect those who cannot receive the flu shot, such as infants and individuals with certain medical conditions, by reducing virus transmission within the community.
- Milder symptoms if flu contracted post-vaccination: Even if the vaccinated individual contracts influenza, the symptoms tend to be less severe, resulting in a faster recovery.
- Economic benefits of vaccination: By preventing illness and reducing absenteeism, the flu shot contributes to economic savings and decreased strain on healthcare resources.
Economically, the flu shot's ability to reduce absenteeism translates to fewer lost workdays, mitigating productivity losses. The United States experiences approximately 111 million lost workdays annually due to influenza, resulting in billions of dollars in lost productivity. Vaccination alleviates this burden, offering a cost-effective strategy for both individuals and employers to maintain a healthy workforce.
Community-wide vaccination efforts enhance herd immunity, bolstering public health by minimizing the spread of influenza. This collective immunity is vital for protecting those who are unable to be vaccinated, effectively curbing outbreaks and safeguarding the most vulnerable members of society. By participating in annual flu vaccination, individuals contribute not only to their well-being but also to the broader health of their community.
Potential Side Effects and Risks of the Flu Shot
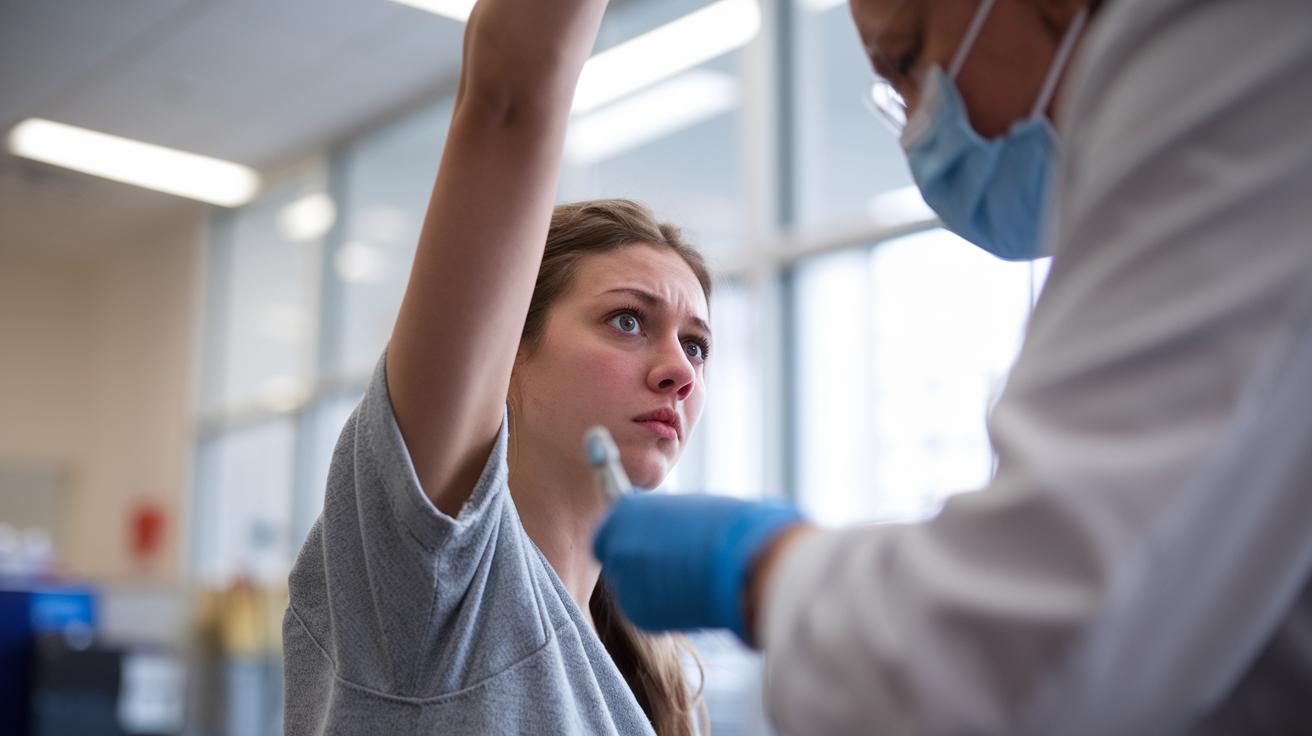
Common side effects of the flu shot are generally mild and manageable, with most individuals experiencing only minor discomfort. These include soreness at the injection site, low-grade fever, and muscle aches, which typically subside within a day. Such reactions are a normal response as the body builds immunity to the influenza virus.
| Side Effect | Duration | Management Tips |
|———————–|————|—————————–|
| Soreness at injection | 1 day | Apply a cold compress |
| Low-grade fever | 1 day | Use over-the-counter pain relievers |
| Muscle aches | 1 day | Rest and stay hydrated |
| Headache | 1 day | Stay hydrated, rest |
| Fatigue | 1 day | Ensure adequate rest |
While the flu shot is predominantly safe, there are rare but severe reactions that warrant attention. Severe allergic reactions, although uncommon, can occur and typically manifest shortly after vaccination. These reactions might include difficulty breathing, swelling, or a rapid heartbeat, and require immediate medical attention.
Another rare risk is the development of Guillain-Barré syndrome (GBS), a condition where the immune system attacks the nerves, potentially leading to muscle weakness and paralysis. However, the incidence of GBS related to flu vaccination is extremely low, estimated at approximately one or two additional cases per million flu shots administered. The benefits of vaccination, in terms of preventing influenza and its complications, significantly outweigh these rare risks. Medical professionals are trained to manage such reactions promptly, ensuring patient safety during and after vaccination.
Cost and Accessibility of the Flu Shot

Is the flu shot covered by insurance? Most insurance plans provide coverage for the flu shot, making it accessible at minimal or no cost to the insured. Clinics and pharmacies frequently offer vaccinations at reduced prices, ensuring broad access to this crucial preventive measure. For individuals with insurance, the cost is typically absorbed by the plan, facilitating widespread immunization efforts.
Where can one get a flu shot? Common locations for receiving a flu shot include:
- CVS Pharmacy
- Walgreens
- Target
How much does the flu shot cost without insurance? The cost of a flu shot can fluctuate significantly for those without insurance, depending on the provider. Prices may range from approximately $20 to $70, influenced by the type of vaccine and the location where it is administered. Some clinics and pharmacies offer promotions or discounts to make the vaccine more affordable for the uninsured. Additionally, community health centers and public health departments may provide the vaccine at no cost or on a sliding scale, further broadening accessibility to all individuals, regardless of their insurance status.
Timing and Best Practices for the Flu Shot

When is the best time to get the flu shot? The ideal timing for receiving the flu shot is early in the season, preferably in September or October. This recommendation is based on the onset of flu season, which typically begins in October and can extend through May. Early vaccination is crucial to allow ample time for immunity to develop before the flu becomes widespread in the community. Administering the vaccine early ensures individuals are protected during the peak months of flu activity.
- Rest after vaccination
- Hydration to alleviate mild side effects
- Monitoring for any adverse reactions
What is the timeline for developing immunity after receiving the flu shot? Immunity from the flu vaccine takes approximately two weeks to develop post-vaccination. During this period, the body produces antibodies in response to the inactivated virus present in the vaccine. These antibodies are vital for protecting against the strains of the flu virus circulating in the current season. Early vaccination is encouraged to maximize protection before flu activity escalates. By ensuring timely vaccination, individuals can substantially reduce their risk of contracting the flu and experiencing severe symptoms.
Final Words
Understanding the flu shot's effectiveness highlights its role in mitigating influenza risks across demographic groups. The flu vaccine's ability to reduce complications, support herd immunity, and lessen economic burdens underscores its importance. While common side effects are typically mild, the potential for rare reactions remains minimal. Accessibility and coverage ensure the flu shot is widely available, reinforcing its value.
Ultimately, determining if the flu shot is worth it lies in its proven capacity to protect individuals and communities alike, making it a vital preventive measure each flu season.
FAQ
What should be avoided after getting a flu shot?
Avoid strenuous activities and excessive alcohol consumption post-vaccination, as these can exacerbate mild side effects like fatigue. It's also advisable to monitor for any adverse reactions and consult a healthcare provider if needed.
What are the benefits and disadvantages of the flu shot?
The flu shot reduces the risk of flu and complications, decreases sick days, and contributes to herd immunity. Disadvantages may include mild side effects, such as soreness or fever, and rare severe allergic reactions.
Does the flu shot weaken your immune system?
The flu shot does not weaken the immune system. It helps build immunity against specific influenza strains, reducing the likelihood of contracting the flu and associated severe complications.
What are valid reasons to decline the flu vaccine?
Valid reasons to decline include severe allergies to vaccine components and a history of serious reactions. It is essential to discuss potential risks with a healthcare provider if unsure.
When is it too late to get a flu shot?
Flu vaccination is advised before flu season peaks, typically by the end of October. However, getting vaccinated later can still provide protection, as flu season can extend into May.
What are the typical side effects of the flu shot?
Common side effects include mild soreness at the injection site, low-grade fever, and muscle aches that generally resolve within a day or two.
How effective is the flu vaccine by age?
Flu vaccine effectiveness varies: children often have robust responses, adults typically experience moderate effectiveness, and seniors might see reduced but still beneficial efficacy.
Is feeling sick two weeks after a flu shot usual?
Feeling mild symptoms is common shortly after vaccination, but if symptoms persist or worsen, consulting a healthcare professional is recommended to rule out other causes.
Is getting a flu shot worthwhile?
The flu shot is a worthwhile preventive measure, significantly lowering flu-related risks and enhancing community protection through herd immunity.
How effective is this year's flu shot?
The effectiveness of this year's flu shot can vary based on the match with circulating virus strains. Updated vaccines typically provide substantial protection and are regarded as the best preventive strategy.